 Cognitive behavioural therapy (CBT) is a psychological treatment that can help with anxiety and depression, as well as some other problems.
Cognitive behavioural therapy (CBT) is a psychological treatment that can help with anxiety and depression, as well as some other problems.
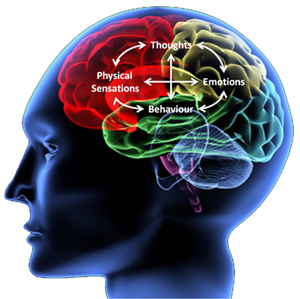
CBT is a modern, evidence-based, and highly effective psychotherapeutic approach, aimed at solving problems related to dysfunctional emotions, behaviours and thoughts (‘cognitions’) through a set of systematic procedures. Many CBT treatment programs for specific disorders have been evaluated for efficacy and most evidence favours CBT over other approaches such as psychodynamic treatments. The UK National Institute for Health and Clinical Excellence (NICE) also recommends CBT as the treatment of choice for a number of mental health difficulties, including post-traumatic stress disorder, OCD, other anxiety disorders, bulimia nervosa, and clinical depression. There is also good empirical evidence that CBT is effective for the treatment of a variety of problems, including mood, anxiety, personality, eating, substance abuse, and psychotic disorders.
CBT was primarily developed through a merging of behaviour therapy with cognitive therapy, and this history is reflected in its current practice, as it encompasses a range of techniques derived from the two approaches. For anxiety disorders, the key technique is often in vivo exposure, sometimes coupled with other techniques such as response prevention (in OCD) and cognitive restructuring (in social anxiety). While highly systematised, CBT practice is flexible enough to accommodate a diversity of therapeutic approaches in order to fit the needs of the patients, and in fact encourages an idiosyncratic ‘model’ of behaviour to be developed for each patient.
For more on CBT see this wikipedia page, and this page on the UK’s NHS website.
